Factoring in Frailty
September 3, 2020

 Contributed by:
Contributed by:
Drs Marjan Abbasi and Sheny Khera
(Click for bio)
Case
Anne is 82 years’ old. She visits her physician to discuss her health concerns of low energy, confusion, and feeling shaky and dizzy. Anne has been slowing down and uses a walker now. Her husband manages the housework and finances while home care provides her with bath assist and medication management. Anne has Type 2 diabetes, hypertension, dyslipidemia and urinary incontinence. Her medications include metformin, gliclazide, sitagliptin, hydrochlorothiazide, ramipril, rosuvastatin, lansoprazole and mirabegron. Her blood pressure in office was 110/60 lying dropping to 82/52 standing and her recent A1C was 6.5.
Issue
Older adults are a heterogeneous population and chronologic age is not synonymous with biologic age.1 Many older adults are functionally independent managing their chronic conditions and thriving in their communities, but others, like Anne, may be facing threats to their independence and are at high risk of adverse events like falls, going to ER, admission to hospital or requiring an alternate level of care. Optimization of seniors’ care, including therapeutic decision-making, must weigh the potential benefit versus harm in the context of overall health – not just based on chronologic age alone; and the significance of this in older adults, like Anne, may be greater given their health is already tenuous (i.e., frailty).2
How do we address Anne’s complex health issues, balancing her frailty and targets of therapy?
Background
Frailty is defined as a heightened state of vulnerability to stressors and can be used clinically to predict likelihood of adverse outcomes.3 Although the prevalence of frailty increases with age, it is not based on age alone. More than 1.2 million Canadians are living with frailty. This includes 16% of people older than 65 years and as many as 52% aged 85 years and older.4 Frailty is multidimensional and is determined by assessing a person’s interrelated biological, psychological and social aspects of life and their ability to respond to and recover from stressors.5
In fact, it is in part due to their higher probability of incurring adverse outcomes that many older adults living with frailty are excluded from clinical trials. The result is that clinicians often must rely on guidelines developed based on healthy individuals. This indiscriminate application to older adults with frailty may lead to limitations to the appropriate treatment of this vulnerable group. Moreover, most guidelines only focus on a single disease, without addressing the vulnerability of older adults with multiple concomitant conditions.6
Applying the lens of frailty thus provides a pragmatic strategy to objectively assess an older person’s risk and avoid the pitfalls of ageism. Understanding frailty can offer older adults choices in line with their objective level of frailty and mitigate against age discrimination for those who are not frail. Decisions about therapies should carefully weigh the individual’s frailty against the potential for benefit and harm from treatment. For example, this may mean exploring less invasive options or anticipating/mitigating potential adverse events while proceeding with treatment. Therefore, factoring in frailty when applying guidelines and treatment targets to older adults is imperative.6
Recognizing Frailty
Comprehensive geriatric assessment (CGA) is the standard process to assess multiple key components of frailty using an interdisciplinary team. However, in routine clinical practice, including primary care, CGA is time consuming and impractical. Several validated tools exist that can be used to quickly recognize and measure frailty.7 The Canadian Frailty Scale (CFS) is a simple visual and practical tool based on the Canadian Study of Health and Ageing8,9 and can be used at the point of care by clinicians familiar with their patients. The CFS categorizes frailty based on physical and functional indicators of health such as cognition, function and mobility with scores that range from 1 (very fit) to 9 (terminally ill).6 Patients with moderate to severe stages of frailty will benefit from the more comprehensive assessment and shared decision-making between the clinician, patient and caregivers. Conversations should focus on patient preferences, medical comorbidities, life expectancy, treatment goals and an appropriate balance between risks and benefits.
Evidence on Frailty and Diabetes
Optimal glycemic control is a cornerstone of diabetes management and A1C values > 7.0 % are associated with increased risk of macro and microvascular complications. However, decision analysis suggests that in patients with multi-morbidity, high functional dependency and reduced life expectancy (i.e., those with moderate-to-severe frailty), the benefit of intensive glycemic control is minimal at best for microvascular complications and does not reduce cardiovascular events or mortality.10 In the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study,11 overall mortality was increased in older adults with longstanding diabetes and multiple comorbidities. Even the final analysis from the ACCORD-MIND sub-study, intensive glycemic control did not preserve brain volume nor alter cognitive outcomes, so intensive glycemic control is not advisable in individuals with frailty.
Diabetes Canada and other international guidelines are recognizing the role of frailty and have shifted focus on functional dependency and life expectancy to determine target A1C. Diabetes Canada uses CFS to illustrate the level of frailty and functional dependency. Based on the Diabetes Canada clinical practice guideline: (Figure 1)
|
Clinical Frailty Scale (CFS) Score |
Functional status |
Acceptable Target A1C (%) |
Preprandial value (mmol/L) |
Postprandial value (mmol/L) |
|
1-3 |
Independent |
≤7.0 |
4-7 |
5–10 |
|
4-5 |
Functional dependency |
7.1–8.0 |
5–8 |
<12 |
|
6-8 |
Higher level of functional dependency/moderate frailty |
7.1-8.5 |
6–9 |
<14 |
In people who are terminally ill or at the end of life (CFS 9), an A1C measurement is not recommended and symptomatic hyperglycemia or any hypoglycemia should be avoided.
Caution is warranted with choice of anti-hyperglycemic medications for older adults, especially with frailty. For example, the risk of severe hypoglycemia may increase substantially with sulfonylureas, in particular glyburide. DPP-4 inhibitors (alogliptin, linagliptin, saxagliptin and sitagliptin) result in similar glycemic control as sulfonylureas but with minimal hypoglycemia. Therefore, DPP-4 inhibitors should be used as second-line therapy to metformin over sulfonylureas. Vitamin B12 should be checked periodically in patients on metformin as well as there may be an association with lower levels of Vitamin B12.10
The ACCORD study demonstrated in type 2 diabetic patients at high risk of CV events that more intensive control of blood pressure (systolic BP <140 mmHg vs. <120 mmHg) did not significantly improve CV outcomes but rather resulted in more side effects.12 Hypertension Canada, collaboratively with Diabetes Canada suggest a target BP of <130/80 mmHg in older diabetic patients who are functionally independent and have a life expectancy of greater than a decade. However, in those with functional dependency, orthostasis or limited life expectancy, individualized BP targets should be considered.10 The American Diabetes Association13 and the International Diabetes Federation14 suggest BP < 140/90 and 150/90 for very frail people with poor health.
Back to the Case
According to the CFS Anne has a score of 6 or moderate frailty. Anne’s symptoms are consistent with hypoglycemia. She is on three anti-hyperglycemic medications and has an A1C of 6.4. This stringent glycemic control is likely causing her episodes of hypoglycemia. According to Diabetes Canada guidance, a target A1C of 7.1-8.5% is acceptable. Anne is also on gliclazide, a sulphonylureas that, at her age also places her at increased risk of hypoglycemia. It was therefore decided to discontinue her gliclazide, repeat her A1C in three months and check her Vitamin B12 as she continued on the metformin. For her blood pressure, it was decided to discontinue her hydrochlorothiazide due to her symptomatic orthostasis and her overall frailty. She will likely benefit from a more liberal target blood pressure.
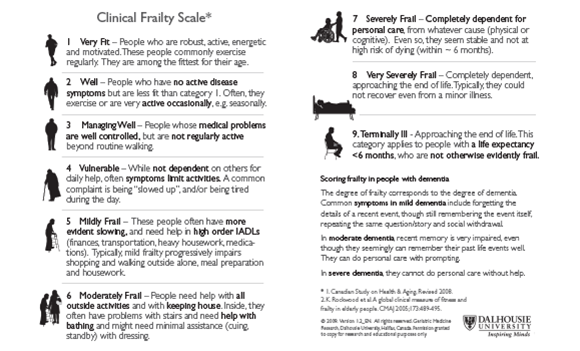
The Canadian Study of Health and Aging (CSHA) Clinical Frailty Scale 8,9
References
- Volpe M, Battistoni A, Rubattu S, Tocci G. Hypertension in the elderly: which are the blood pressure threshold values?. Eur Heart J Suppl. 2019;21(Suppl B):B105‐B106. doi:10.1093/eurheartj/suz023
- Mallery LH, Allen M, Fleming I, et al. Promoting higher blood pressure targets for frail older adults: a consensus guideline from Canada. Cleve Clin J Med. 2014;81(7):427‐437. doi:10.3949/ccjm.81a.13110
- Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people [published correction appears in Lancet. 2013 Oct 19;382(9901):1328]. Lancet. 2013;381(9868):752‐762. doi:10.1016/S0140-6736(12)62167-9.
- Hoover M, Rotermann M, Sanmartin C, Bernier J. Validation of an index to estimate the prevalence of frailty among community-dwelling seniors. Health Rep. 2013;24(9):10‐17.
- Puts MTE, Toubasi S, Andrew MK, et al. Interventions to prevent or reduce the level of frailty in community-dwelling older adults: a scoping review of the literature and international policies. Age Ageing. 2017;46(3):383‐392. doi:10.1093/ageing/afw247
- Mallery LH, Ransom T, Steeves B, Cook B, Dunbar P, Moorhouse P. Evidence-informed guidelines for treating frail older adults with type 2 diabetes: from the Diabetes Care Program of Nova Scotia (DCPNS) and the Palliative and Therapeutic Harmonization (PATH) program. J Am Med Dir Assoc. 2013;14(11):801‐808. doi:10.1016/j.jamda.2013.08.002
- Abbasi M, Rolfson D, Khera AS, Dabravolskaj J, Dent E, Xia L. Identification and management of frailty in the primary care setting [published correction appears in CMAJ. 2019 Jan 14;191(2):E54]. CMAJ. 2018;190(38):E1134‐E1140. doi:10.1503/cmaj.171509
- Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489‐495. doi:10.1503/cmaj.050051
- Dalhousie University Faculty of Medicine. Geriatric medicine research. Clinical Frailty Scale. Updated 15 July 2015. Available from: http://geriatricresearch.medicine.dal.ca/ clinical_frailty_scale.htm [accessed 17 December 2017].
- Diabetes Canada Clinical Practice Guidelines Expert Committee, Meneilly GS, Knip A, et al. Diabetes in Older People. Can J Diabetes. 2018;42 Suppl 1:S283‐S295. doi:10.1016/j.jcjd.2017.10.021
- Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545‐2559. doi:10.1056/NEJMoa0802743
- ACCORD Study Group, Cushman WC, Evans GW, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1575‐1585. doi:10.1056/NEJMoa1001286
- Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes Care. 2012;35(12):2650‐2664. doi:10.2337/dc12-1801
- International Diabetes Federation. Managing older people with type 2 diabetes global guideline. Brussels, Belgium: International Diabetes Federation (IDF), 2013 http://www.idf.org/sites/default/files/IDF-Guideline-for-older-people-T2D.pdf.
