Flawed data equals flawed decision-making
February 14, 2020
Dear Members:
In my President’s Letter last Friday, I shared our negotiations objectives and what we consider to be key requirements for reaching a deal with government:
- Better information – government is using misleading physician payment figures
- Clear vision required – a lot of ideas out there, they need to be brought into focus
- Provincial physician compensation strategy – essential for true system improvement
- A way to deal fairly with physician supply and control practitioner ID numbers
Today I would like to focus on the first requirement: better information.
Many of you have contacted me in the past few months. You have told me that the data on patient outcomes and physician compensation presented by government is not congruent with your own knowledge and experience. I want to thank you for reaching out and for sharing your stories and lived experiences working within the system. They are indeed much different than the picture government is painting.
Flawed data and a lack of understanding
In our profession, we are obligated to obtain accurate data and assessments to provide high quality care for our patients. It is clear that government does not adhere to the same standards.
The data used to justify several of Alberta Health’s consultation proposals is inherently flawed. The consultation proposals, which AH has now made public and the AMA has responded to, have resulted in an outpouring of profound concern by our rural and urban family medicine colleagues. What is most concerning is the fact that there seems to be zero recognition of the negative consequences to patient care that will ensue if these proposals are enacted in their current form. In what is still a public system, not paying physicians properly to spend time with their patients is directly denying care to Albertans.
On another front, arbitrary cuts have been made to the Alberta Health Services physician on-call program, affecting both rural and urban physicians. No clinical data to justify the cuts has been offered, and there is no evidence that an impact analysis was performed. Here again, government is completely failing to recognize the direct negative impact these decisions have on patient care.
AH consultation proposal 8 calls for elimination of AHS clinical stipends. The AMA received a letter from AHS on December 17, 2019 indicating that out of a total of 247 stipend arrangements, 63 were being targeted for elimination by March 31, 2020. This affects 967 practitioners and approximately $16.8M in physician compensation.
I have heard from and met with many of our members on this issue. No one is aware of any analysis undertaken to address the potential impact on the clinical services provided to patients by our AHS-based physician colleagues.
A transition to clinical Alternative Relationship Plan’s (ARP’s) has been put forward as a solution. The AMA has been a pioneer in encouraging alternate payment models for years, but we need to align the model with what patients need. Even if all of the factors were in place to move a large number of physicians over to an ARP, Alberta Health does not have the capacity to make this happen. We have heard from numerous physicians who have been waiting years to get an ARP established. What will happen to patients in the meantime? Sadly, government is again demonstrating their lack of system understanding as this solution fails to recognize that ARP’s cannot possibly be set up quickly enough to prevent a serious degradation to vital services.
The recent Ernst and Young AHS report made 57 recommendations for cost savings. Regrettably, the data used to justify the recommendations was often misleading and erroneous. Some section leaders have already provided critiques of the report as it relates to their work:
- Letter from Section of Diagnostic Imaging to AHS
- Section of Laboratory Physicians' submission, February 2020 edition of Section News
Physician Payments in Alberta
One of our main areas of concern relates to physician payments and government’s lack of understanding in this area.
Beginning with the MacKinnon report, government has released a number of concerning and disparaging statements comparing Alberta physician payments with those in other provinces.
The AMA recently engaged Invictus Analytics & Strategy (an independent consultancy that government hired during the negotiation of two previous AMA agreements) to develop a principles-based approach to benchmark Alberta with relevant comparator provinces on two key measures:
- Average clinical payments to physicians
- Physician payments per capita
One of the government’s favorite statistics to quote from the MacKinnon report claims that average clinical payments to physicians in Alberta are 35.2 percent higher than comparator provinces of BC, Ontario and Quebec. This claim is based solely on Canadian Institute for Health Information (CIHI) fee-for-service comparisons for 2016/17, and does not account for differences in ARP earnings, nor important concessions made by Alberta physicians in recent master agreements. The comparator provinces chosen also do not reflect current labour market dynamics, such as interprovincial physician migrations.
When appropriate adjustments are made – including adjustments to recognize recent increases negotiated in other provinces – Alberta’s physician compensation is actually in line with comparator provinces. The graphic below illustrates the elements that the MacKinnon report failed to take into account when drawing conclusions:
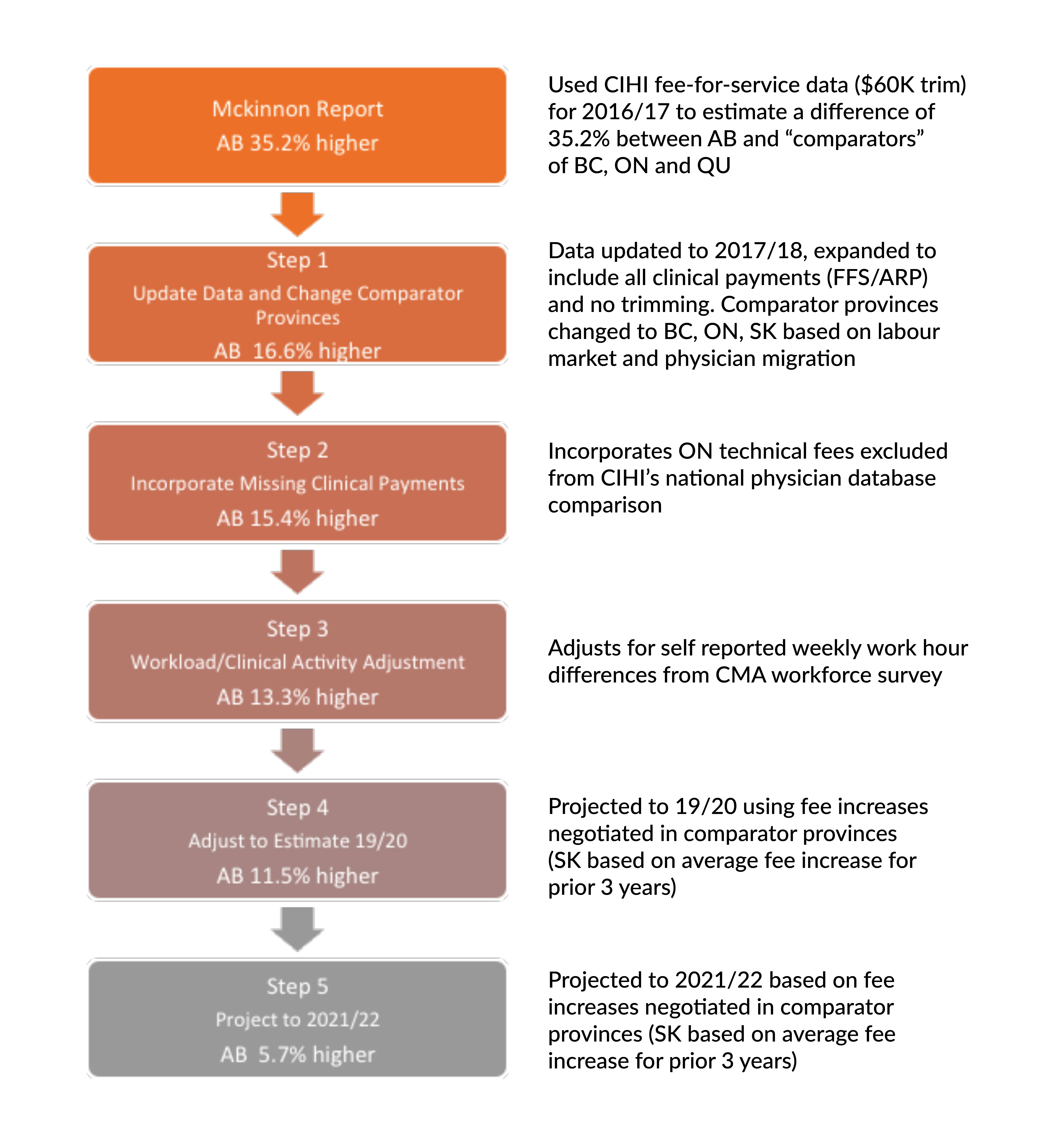 Once proper adjustments are made, Alberta’s average physician compensation is projected to be 5.7 percent higher than our comparator provinces by 2021/22. But again, context matters, which is why it’s important to point out that this projection is based on current status and does not factor in any government cuts (i.e., if consultation proposals are implemented).
Once proper adjustments are made, Alberta’s average physician compensation is projected to be 5.7 percent higher than our comparator provinces by 2021/22. But again, context matters, which is why it’s important to point out that this projection is based on current status and does not factor in any government cuts (i.e., if consultation proposals are implemented).
The AMA’s Economic Realities of Physician Compensation paper demonstrates that wage differences elsewhere in the economy (i.e., among other workers and their interprovincial counterparts) are much higher. In 2017/18, Alberta’s industrial aggregate wage level was 15.4 percent higher than the averages in BC, Ontario and Saskatchewan. As employers themselves, physicians are directly impacted by these higher wages through increased staff/overhead costs.
The independent consultant also demonstrated that the gap in adjusted average clinical payments per capita between Alberta and our comparator provinces will close by 2021/22 due to recently negotiated fee increases in comparator provinces, and expected physician and population growth over the next two years. In fact, by 2021/22 Alberta will fall slightly below the average (-2.5%).
Where we need to go from here
At the negotiating table, the AMA team has recommended that both sides work together to develop appropriate comparisons of physician compensation based on objective sources of information. In order to reach an agreement we have to first agree on the facts we are basing decisions on. There is no question that policy decisions based on flawed data will ultimately be bad for the health care system, physicians and – most importantly – Albertans.
Your comments are welcome in the following ways:
- Communicate with me privately and directly by email if you would like a reply: president@albertadoctors.org.
- Comment publicly below (please be aware that comments are public, i.e., not members-only, even if you are logged in as a member).
In your service,
Christine P. Molnar, MD, FRCPC
President, Alberta Medical Association

5 comments
Commenting on this page is closed.
This comment has been deleted.
This comment has been deleted.
This comment has been deleted.
This comment has been deleted.
This comment has been deleted.