Focus on Parkinson’s disease – Part 2 (advanced disease and psychosis)
May 11, 2023

 Contributed by:
Contributed by:
Joyce Lee MD CCFP COE, BScPharm – View bio
Case
George is 72 and a retired teacher. He has a 10-year history of Parkinson’s disease with motor fluctuations including end of dose wearing off, for which he receives pramipexole and entacapone; and peak dose dyskinesias (involuntary movements), for which he receives amantadine. His non-motor symptoms include REM sleep disorder, constipation and overactive bladder. He presents with six months of visual hallucinations (seeing people and animals in his home), paranoid delusions about his wife, online gambling and cognitive decline. He has lost 20 pounds from excessive exercising which started eight months ago (current BMI of 21).
Patient medical history includes hypertension, anxiety and type 2 diabetes mellitus. He lives with his wife Alice in a bungalow and uses a walker. His medications include:
Table 1
|
|
|
|
|
|
|
|
|
|
|
|
|
Issue
Analyze George’s presentation in context of his medication regimen, disease and risk factors. Suggest appropriate medication changes to improve his symptoms.
Background
The epidemiology of Parkinson’s disease (PD) and its relevance in caring for older adults were reviewed in part 1 of this series.1 As PD progresses, patients experience increasing motor and non-motor complications which impact their quality of life and increase caregiver burden.2,3
Psychosis
Neuropsychiatric symptoms such as psychosis are in particular associated with increased caregiver stress and hospitalization risk.2,4,5 The presence of psychosis should trigger a thorough medical, cognitive and medication assessment.6 Psychosis can develop due to PD dementia, medication side effects, or a combination of both. PD-associated cognitive impairment/dementia is present in more than 75% of patients by eight years.7
After delirium is ruled out and acute medical issues are addressed, the clinician should aim to reduce/stop medications most likely to contribute to psychosis. Anticholinergic medications including OTCs (e.g., dimenhydrinate and antihistamines) should be minimized. Overactive bladder agents with high anticholinergic burden such as oxybutynin and tolterodine should be switched to an alternative such as mirabegron.8,9
As all PD medications could potentially cause psychosis, the ones which are most implicated should be tapered/stopped first. Guidelines recommend the following order (Figure 1) to taper/stop the medications, while monitoring for motor symptom worsening.6 It is important that amantadine and dopamine agonists be tapered as both are associated with withdrawal syndromes.
Figure 1: How to stop/taper PD medications in psychosis
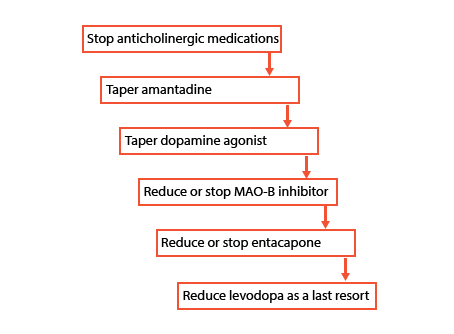
References: Flowchart algorithm from Grimes et al 2019.10
The only antipsychotics which could be used in PD psychosis without motor symptom worsening are quetiapine and clozapine.6 Given clozapine is associated with agranulocytosis and requires extensive blood monitoring, the first line is quetiapine. Where psychosis is severe and endangering self/others, quetiapine can be started at low dose (12.5 mg po hs) and titrated up as tolerated, watching for orthostatic hypotension, QT prolongation and constipation. Quetiapine should NOT be prescribed as a reflexive response to psychosis in PD without attempts to reduce culprit medications.
PD dementia (PDD) is similar in symptomatology to dementia with Lewy bodies (DLB) as they share Lewy bodies as their common pathology. Symptoms include poor/fluctuating attention and level of alertness, vivid visual hallucinations, poor executive function, neuroleptic sensitivity and autonomic features.7,11 Psychosis, behavioural disturbance and function improve with cholinesterase inhibitor (CI) treatment.12 Thus CI (donepezil or rivastigmine) should be offered in PDD,6 considering significant weight loss, low body weight and cardiac conduction deficits (heart block beyond first degree, left bundle branch block) as contraindications. Side effects of CI include GI (nausea, weight loss, diarrhea), cardiac/autonomic (orthostatic hypotension, bradycardia, syncope), and tremor in PDD. A pre- and post-treatment ECG is recommended. Memantine can be used in cases where CI is contraindicated or not tolerated.6
Weight
Weight and muscle loss (sarcopenia) is often the trigger for frailty syndrome in older adults with PD.13,14 Levodopa dosing is weight-based,15,16 thus weight loss triggers a relative levodopa excess, leading to exaggerated side effects, including peak-dose dyskinesias, orthostatic hypotension, impulsivity and psychosis.17 Thus, weight loss should alert the prescriber to reassess PD medication dosing.
Impulse control disorder (ICD)
ICD is defined as the failure to resist an impulse or temptation to perform an act (that is harmful to the person or to others). Risk factors include male sex, younger age, history of ICDs, history of mood disorders (particularly depression), apathy and a family history of ICDs and addiction.18 Dopamine agonists (DAs) such as pramipexole and ropinirole are particularly associated with a higher risk of ICD, compared to levodopa (13% vs. 0.7%).19 ICD can present as gambling, hypersexuality, compulsive hobbyism, eating, buying, punding (repetitive task with no purpose) and increased use of PD drugs. DAs should be avoided in older adults, cognitive impairment and people at risk for ICD.6
Assessment and evidence
George presents with psychosis, cognitive decline and impulse control disorder on a background of PD for 10 years. These symptoms were exacerbated by a 20-pound weight loss, which led to relative excess of dopaminergic dosing and exaggerated side effects. George likely has underlying PDD as well given his duration of PD.
The main culprit medications in this case are tolerodine (anticholinergic), amantadine (anticholinergic property) and pramipexole (dopamine agonist). The following changes are recommended:
- Switch tolterodine to mirabegron 25 mg po daily.
- Reduce amantadine to 50 mg po bid at 7 a.m. and 2 p.m. (Note: this would make dyskinesias worse if there is not concomitant reduction of dopaminergic therapy).
- Concurrently, reduce pramipexole to 0.375 mg po tid for three weeks, then 0.25 mg po tid for three weeks, then 0.125 mg po tid for three weeks, hopefully to stop. (Monitor motor symptoms and for emergence of dysphoria, part of dopamine agonist withdrawal syndrome). If motor symptoms worsen to unacceptable degree, increase levodopa cautiously.
- Quetiapine 12.5 mg po hs could be started for two weeks for distressing psychosis, until the above medication changes take effect.
Once his condition settles, he should be evaluated with cognitive assessment, which would likely find evidence of PD dementia. Cholinesterase inhibitor would be relatively contraindicated due to weight loss, at least until George regains some weight. In the meantime, memantine 5 mg po bid can be considered, titrating to 10 mg po bid, although it is not covered under provincial health plans.
Summary/practice tips
PD dementia and psychosis become more common with longer duration of PD. At this juncture, patients’ dopaminergic regimen should be reassessed and often reduced. Remind the patient and caregiver that the goal of dopaminergic therapy is to improve function; and when cognitive decline, psychosis and impulsivity are present, excessive dopamine worsens neurocognitive symptoms and overall function. Thus, optimization of motor symptoms must be balanced with non-motor symptoms in advanced PD. Quetiapine is sometimes necessary in distressing psychosis but should not be used without an attempt to reduce dopaminergic medications.
Once PD dementia is diagnosed, donepezil or rivastigmine can be offered if not contraindicated, while memantine is a second line option.
References
- Lee J. Focus on Parkinson’s disease – Part 1 | Alberta Medical Association. Optimized Prescribing with Seniors, Jan 2023. Accessed February 24, 2023. https://www.albertadoctors.org/services/media-publications/newsletters-magazines/ops/focus-on-parkinsons-disease-part-1
- Martinez-Martin P, Rodriguez-Blazquez C, Forjaz MJ, et al. Neuropsychiatric symptoms and caregiver’s burden in Parkinson’s disease. Parkinsonism Relat Disord. 2015;21(6):629-634. doi:10.1016/J.PARKRELDIS.2015.03.024
- Gilbert R, Khemani P. Treatment of Advanced Parkinson’s Disease. https://doi.org/101177/0891988720988904. 2021;35(1):12-23. doi:10.1177/0891988720988904
- Oh Y-S, Lee JE, Lee PH, Kim J-S. Neuropsychiatric symptoms in Parkinson’s disease dementia are associated with increased caregiver burden. J Mov Disord. 2015;8(1):26-32. doi:10.14802/jmd.14019
- Lee JW, Mah G, Kalia S, Miyasaki J. Emergency Room visit prevention for older patients with parkinsonism in a Geriatric Clinic. Can J Neurol Sci / J Can des Sci Neurol. Published online November 13, 2020:1-36. doi:10.1017/cjn.2020.253
- Grimes D, Fitzpatrick M, Gordon J, et al. Canadian guideline for Parkinson disease. CMAJ. 2019;191(36):E989-E1004. http://www.cmaj.ca/content/191/36/E989
- Aarsland D, Andersen K, Larsen JP, Lolk A. Prevalence and Characteristics of Dementia in Parkinson Disease. Arch Neurol. 2003;60(3). doi:10.1001/archneur.60.3.387
- Herschorn S, Staskin D, Schermer CR, Kristy RM, Wagg A. Safety and Tolerability Results from the PILLAR Study: A Phase IV, Double-Blind, Randomized, Placebo-Controlled Study of Mirabegron in Patients ≥ 65 years with Overactive Bladder-Wet. Drugs and Aging. 2020;37(9). doi:10.1007/s40266-020-00783-w
- Lozano-Ortega G, Walker DR, Johnston K, et al. Comparative Safety and Efficacy of Treatments for Overactive Bladder Among Older Adults: A Network Meta-analysis. Drugs and Aging. 2020;37(11):801-816. doi:10.1007/S40266-020-00792-9/TABLES/3
- Frank C, Ccfp MD, Fcfp R, Chiu C, Lee J. Parkinson disease primer, part 2: management of motor and nonmotor symptoms. Can Fam Physician. 2023;69(2):91-96. doi:10.46747/CFP.690291
- McKeith IG, Boeve BF, Dickson DW, et al. Diagnosis and management of dementia with Lewy bodies. Neurology. 2017;89(1):88 LP - 100. doi:10.1212/WNL.0000000000004058
- Matsunaga S, Kishi T, Yasue I, Iwata N. Cholinesterase Inhibitors for Lewy Body Disorders: A Meta-Analysis. Int J Neuropsychopharmacol. Published online 2015:1-15. doi:10.1093/ijnp/pyv086
- Tan AH, Hew YC, Lim SY, et al. Altered body composition, sarcopenia, frailty, and their clinico-biological correlates, in Parkinson’s disease. Park Relat Disord. 2018;56:58-64. doi:10.1016/j.parkreldis.2018.06.020
- Peball M, Mahlknecht P, Werkmann M, et al. Prevalence and associated factors of sarcopenia and frailty in Parkinson’s disease: A cross-sectional study. Gerontology. 2019;65(3):216-228. doi:10.1159/000492572
- Müller T, Woitalla D, Saft C, Kuhn W. Levodopa in plasma correlates with body weight of parkinsonian patients. Parkinsonism Relat Disord. 2000;6(3):171-173. doi:10.1016/S1353-8020(00)00005-5
- Nishikawa N, Iwaki H, Shiraishi T, Mukai Y, Takahashi Y, Murata M. Female, aging, difference formulations of DCI, or lower body weight increases AUC4hr of levodopa in patients with Parkinson’s disease. Park Relat Disord. 2020;76:16-20. doi:10.1016/j.parkreldis.2020.05.020
- Tran TN, Vo TNN, Frei K, Truong DD. Levodopa-induced dyskinesia: clinical features, incidence, and risk factors. J Neural Transm. 2018;125(8). doi:10.1007/s00702-018-1900-6
- Pringsheim T, Day GS, Smith DB, et al. Level of Recommendation A Report of the AAN Guideline Subcommittee. Published online 2021. doi:10.1212/WNL.0000000000012868
- Voon V, Hassan K, Zurowski M, et al. Prevalence of repetitive and reward-seeking behaviors in Parkinson disease. Neurology. 2006;67(7):1254-1257. doi:10.1212/01.WNL.0000238503.20816.13
