Understanding Doctors’ Pay
Context Matters: The Facts about Physician Compensation in Alberta
Transparency regarding physician payments is important. An honest conversation about physician payments should include all the facts. Doctors’ gross payments are not their take home pay. Context matters.
Transparent reporting matters
Transparency in reporting how public funds are spent is important. Government already publishes a variety of physician payment information through the Alberta Health Care Insurance Plan Statistical Supplement, including services delivered and number of patients cared for.
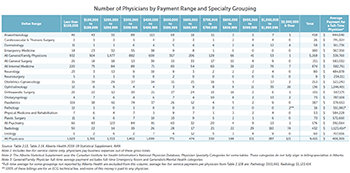
Payment ranges for all physician specialties are already publicly available: (Click to view full size)
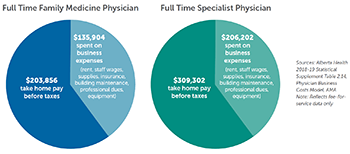
Business expenses are a significant component of every physician’s compensation
On average, 40% of physician billings go directly to covering business related expenses, while some individual physician practices are much higher (up to 75%).
(Click to view full size)
CONTEXT NOTE: The above are typical amounts for family and specialist physician pay and their associated business expenses, but this is not the whole picture. For a more complete picture, please see additional context and examples.
Gross payments are not take home pay
Most Alberta physicians are small business owners. Our offices are a major part of the infrastructure of the health care system.
 As with any business, there are costs associated with running a medical practice. Physicians pay for these business costs out of the fees they charge the health care system for the services they provide to patients (i.e., the dollar amounts you would see on a gross payment Sunshine List).
As with any business, there are costs associated with running a medical practice. Physicians pay for these business costs out of the fees they charge the health care system for the services they provide to patients (i.e., the dollar amounts you would see on a gross payment Sunshine List).
Physicians are responsible to pay for:
- Staff they hire and the corresponding employee benefits
- Professional services to support their practice, such as billing support or accountants
- Rent, utilities, office supplies, equipment, office maintenance and improvements, etc.
- Professional licensing and business insurance, plus an increasing portion of liability insurance
Then they pay themselves a salary (and pay their income taxes).
Business expenses matter
 The amount needed to cover expenses varies greatly, i.e., physicians that practice in the community (those that maintain an office outside of the hospital) incur higher business expenses than those that provide services only in hospitals.
The amount needed to cover expenses varies greatly, i.e., physicians that practice in the community (those that maintain an office outside of the hospital) incur higher business expenses than those that provide services only in hospitals.
Important to note that physicians DO NOT receive:
- Pensions
- RRSP benefits
- Health and dental benefits
- Life and disability insurance
- Sick pay
- Reimbursement for ongoing medical education, necessary to maintain their licenses
- Reimbursement for additional costs such as personal protective equipment and sanitizing supplies that have become necessary due to the pandemic
Like most other small business owners, physicians are responsible for these expenses.
Work hours matter
Physicians do not have a 9-5 job. Often when they have finished seeing their patients, there are multiple follow-up requirements needed to complete the initial visit (in-person or virtually).
- 7,988 Alberta physicians worked one or most statutory holidays in 2018-19
- 4,539 Alberta physicians provided overnight/after-hours services in 2018-19
- A 2019 Canadian Medical Association survey showed Alberta physicians work approximately 50 hours per week + 25 hours for on call service
Physician burnout in Alberta is an ongoing concern.
Physician training matters
Physicians train longer than most workers in the economy – a lot longer for some specialties and subspecialties.
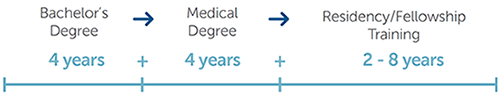
= Up to 16 years total post secondary training for some + annual education required to maintain license
= Late entry in the job market
= Shortened career (often 30 years or less) in which to pay off hefty student loans, earn income and save for retirement
Supporting the economy matters
 Radiologist community clinics alone directly employ over 2,300 Albertans.
Radiologist community clinics alone directly employ over 2,300 Albertans.
Physicians hire other service providers, including nurses, nurse practitioners, medical office assistants, clinic managers, dietitians, physiotherapists, accountants, tradespeople, technicians, etc.
Alberta’s Recovery Plan states that “Alberta’s small and medium enterprises are the backbone of our economy and they will be integral to our recovery.”
Physician offices are an important part of that backbone.
Let’s get back to what matters
It’s about more than physicians’ gross billing. Let’s get back to the table to negotiate a new agreement between the AMA and the Government of Alberta. Our health care system desperately needs the stability that can only come from working together.
This is what Albertans need and deserve.
Patient counts matter
Discrete patient counts provide the number of different patients a physician sees, but do not account for the number of services each of those patients receives. Put more simply, some patients require more services from a physician, or more complex services, and are therefore more expensive to care for. This is why discrete patient counts can provide a skewed perspective. As examples:
- Family physicians providing continuous, comprehensive care within a Patient’s Medical Home style practice to a population of patients with greater co-morbidities may see fewer patients in one year than a family physician providing episodic or symptomatic care to a population of patients with fewer co-morbidities.
- Specialist physicians that are actively managing a greater proportion of complex patients with chronic diseases such as renal failure, cancer, or cardiac complications will see fewer patients in one year (and will therefore appear to have higher costs per patient) than those who provide care to patients with acute episodic conditions that are more likely to appear (for example) in the Emergency Room.
Business expenses matter
Additional context and examples
All physicians in Alberta incur business costs and the amounts vary from specialty to specialty and often practice to practice within specialties. We think it’s important to provide some real-life insight from physicians who are incurring these costs as they care for Albertans.
The following testimonials offer a look into the business costs associated with practicing different kinds of medicine in Alberta:
Radiology
A typical radiology clinic in the community employs 15-20 people and costs $3,000,000 or more to build and equip with high-tech medical imaging equipment and IT systems. All of this must be deducted from the doctor’s gross billings to Alberta Health, not to mention the rent, medical supplies, personal protective equipment for staff and patients, special licensing costs, and so on.
The majority of the fees paid to these doctors – around 70% but sometimes more – goes first to cover the salaries for their employees and these other large expenses. The more time over the year that a radiologist is scheduled to work in these clinics instead of in the hospital, the more their total billings will generally be, but they would also be paying proportionally more of these expenses within the system. Gross fee-for-service billing does not tell you much about the actual take-home pay of individual doctors, and neither does the variation in billing.
Radiology clinics collectively lease over 600,000 square feet of specialized space at over 125 clinic locations in urban and rural Alberta. They operate more than 600 installations of high-tech medical equipment on behalf of the public system. The capital investment represented by this is in the $400,000,000 range, which is a huge investment in the public health care system and the Alberta economy. The majority of imaging studies in Alberta are done in these clinic facilities already, not AHS, with minimal waitlists for services and extremely high patient satisfaction. Overall, approximately 70% of fee-for-service payments to radiologists go to covering these costs within the public system.
Dr. Robert Davies | President, Alberta Society of Radiologists | President, AMA Section of Diagnostic Imaging
Ophthalmology
Gross revenues are not reflective of a physician’s actual remuneration and include all staff salaries and benefits, as well as infrastructure and operating costs of clinics. Ophthalmologists require highly specialized, meticulous and delicate equipment and highly-skilled staff to assist them.
An ophthalmology office has both large administrative costs and specialized technical requirements. This technical medical infrastructure, built and paid for by the ophthalmologist, replaces many in-hospital diagnostic services that used to be funded within hospital budgets. There is no longer enough public infrastructure to meet the need for vision-saving care for Albertans. It should be noted that a large range of practice types and volumes exist within ophthalmology, and there is great variability in billings. Higher-volume practices, with higher technical requirements, tend to incur higher overhead costs proportionate to higher gross billings. On average, an ophthalmologists overhead costs are 55% of their total billings. Detailed independent studies in 2014-15 revealed overhead costs averaging from $880,000 per physician for group practices, and $1.6 million per year for a solo practitioner in one high-volume subspecialty.
High-volume practices are crucial to meet the needs of Albertans. Compared to other countries, Canada has a shortage of these specialists. The International Council of Ophthalmology reports that Canada has only 32 ophthalmologists for every million residents, roughly half the similar service available in the United States. Canadian ophthalmologists serve about twice as many patients as their U.S. counterparts.
Dr. Stephanie Dotchin | President, Eye Physicians and Surgeons Association of Alberta | President, AMA Section of Ophthalmology
Dermatology
The Section of Dermatology has already studied the cost of practice and would like to share the following information:
There are currently 58 dermatologists practicing in Alberta. Those 58 dermatologists see approximately 450,000 Albertans each year and provide over 750,000 health care services to those patients.
On average, our annual gross revenue is $911,736 per full-time, fee-for-service dermatologist. These dermatologists have high overhead – business costs – averaging $487,778 per full time physician. That equates to more than half (53.5%) of our total compensation every year.
These figures represent averages for all dermatologists and it’s important to keep in mind that there can be some variation in revenues and the number of services provided. For example, dermatology surgeons providing life-saving cancer surgery will see fewer patients, but will bill more per patient as their work entails multiple procedures on the same patient.
Dr. Gordon Searles | President, AMA Section of Dermatology
Family Medicine
Prior to the COVID-19 pandemic, overhead expenses to run an urban family medicine practice in Alberta were typically 40% or a little more. With the additional expense of providing personal protective equipment for all staff and patients, this figure will be higher this year.
On average, a family medicine clinic employs approximately one staff member per physician, which works out to about 6,000 direct employees in total. Within a Primary Care Network clinic, the staffing costs increase substantially due to the extra support staff hired to care for patients within a Patient’s Medical Home Model. These clinics often hire several support staff and other health professionals such as nurses, dieticians, physiotherapists, health educators, etc.
Dr. Craig Hodgson | President, AMA Section of Family Medicine
Pediatrics
In addition to caring for patients in the community, pediatricians also provide specialty services in AHS facilities for many complex patient populations across Alberta and acute 24/7 coverage in hospitals. These services are essential for safe care of the most vulnerable members of our society, including: children with cancer; severe physical and cognitive disabilities; life altering or life limiting heart conditions; children in foster care with complex medical needs; or victims of child abuse.
Even when pediatricians are working in AHS hospital facilities, they still continue to pay for their overhead expenses in their community clinics. They need to pay for their rent, insurance and office staff. These overhead expenses can run between 30-40%.
Dr. Sidd Thakore | Secretary-Treasurer, AMA Section of Pediatrics
General Psychiatry
In psychiatry, our overheads can be simpler than many of our other colleagues, but it still remains substantial. For psychiatrists practicing in the community, our overheads will often include leased office space, IT infrastructure and, on average, one full-time administrative assistant for every 2-3 psychiatrists.
On top of that, many psychiatrists don’t just work full-time in a community practice or in a single location. For example, I spend half of my time managing in-patients at a hospital, and 1 to 1.5 afternoons per week in an AHS community practice. While I am at those locations, I’m still obliged to cover my overhead costs at my other general practice. As you can imagine, my practice has to be available for messages, crisis management, the management of referrals and other physician-to-physician and physician-to-patient communications.
Depending on the specific set up of a practice, overhead costs can easily range from 20% to 40% of our total gross billings. And this would be based on pre-COVID numbers. Many psychiatrists have seen a reduction (in the neighborhood of 10-20%) in their fees since the onset of COVID. This is because most virtual codes do not account for higher complexity patients, and group therapy based practices have essentially come to a stop due to the pandemic because we lack an equivalent billing code to provide this service.Nonetheless, our overheads have generally remained fully in place.
Definitely, what we bill, is not what any of us take home.
Dr. Sudhakar Sivapalan | Member-at-Large, AMA Section of General Psychiatry
Pathology
Laboratory physicians include multiple sub-specialty physicians, including anatomical pathologists, general pathologists, medical microbiologists and hematopathologists/transfusion medicine physicians.
In Alberta, laboratory physicians are paid on a 4-tier grid system that ranges from $354,000 to $412,000 per year. Movement along the grid is based on the years of service to the organization. More than 90% of laboratory physicians do not bill fee-for-service through the Schedule of Medical Benefits. The information gleaned from the available Alberta Health statistical supplement is grossly inaccurate because laboratory physicians moved into a quasi-alternative relationship plan type remuneration model many years ago and this reality has not been captured.
Alberta continues to struggle to attract laboratory physicians despite an increase in demand due to an aging population and the increasing complexity of medicine. Laboratory physicians are like the air we breathe; everywhere for everyone, all the time. Until it’s gone.
Dr. Brinda Balachandra | President, AMA Section of Laboratory Physicians | President, Alberta Society of Laboratory Physicians
Rural Medicine
Rural doctors give so much to the communities we call home. We are responsible for looking after our patients in all settings: clinic, hospital, emergency department, or even at their houses. Many of us deliver babies, offer surgery or anesthesia and/or provide a host of other specialized skills so that patients can get their care locally. This 24/7 coverage usually falls to a small number of physicians, meaning that we work long hours (60-80+ per week) and give up our family and personal time to serve our population. Our clinic in Pincher Creek has adopted a “Patient’s Medical Home” model, which means a higher staff to physician ratio of 3:1. Although this means we pay higher overhead (up to 50% on clinic billings), this model allows us to provide better patient care with the added bonus of creating more jobs for our friends, neighbours and, yes, our patients. I don’t think the Sunshine List will matter much to our fellow rural community members. They know how hard we work and how valuable it is to have all the services we provide available in their home community.
Dr. Samantha Myhr | President, AMA Section of Rural Medicine